Senses are the physiological methods of perception. The senses and their operation, classification, and theory are overlapping topics studied by a variety of fields. Sense is a faculty by which outside stimuli are perceived.
Chemoreception
The senses of Gustation (taste) and Olfaction (smell) fall under the category of Chemoreception. Specialized cells act as receptors for certain chemical compounds. As these compounds react with the receptors, an impulse is sent to the brain and is registered as a certain taste or smell.
Gustatory System
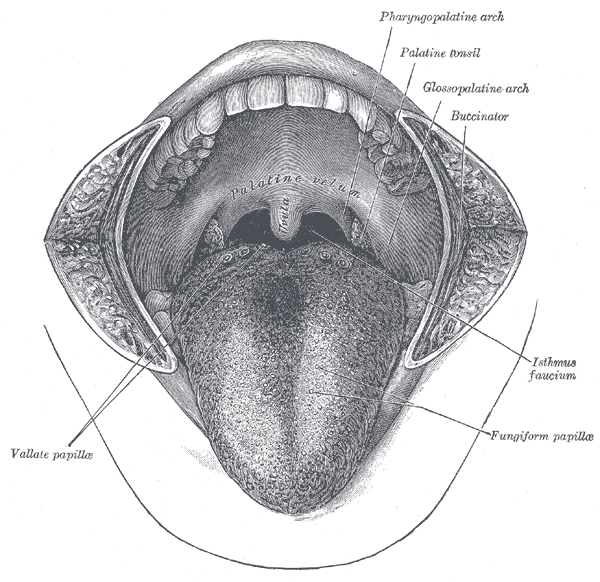
In humans, the sense of taste is transduced by taste buds and is conveyed via three of the twelve cranial nerves. Cranial nerve VII, the facial nerve, carries taste sensations from the anterior two thirds of the tongue (excluding the circumvallate papillae, see lingual papilla) and soft palate, crainal nerve IX the glossopharyngeal nerve carries taste sensations from the posterior one third of the tongue (including the circumvallate papillae) while a branch of the vagus nerve carries some taste sensations from the back of the oral cavity (i.e. pharynx and epiglottis). Information from these cranial nerves is processed by the gustatory system. Though there are small differences in sensation, which can be measured with highly specific instruments, all taste buds can respond to all types of taste. Sensitivity to all tastes is distributed across the whole tongue and indeed to other regions of the mouth where there are taste buds (epiglottis, soft palate).
Papilla
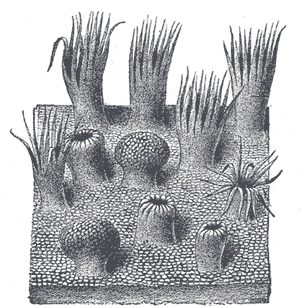
Papilla are specialized epithelial cells. There are four types of papillae: filiform (thread-shape), fungiform (mushroom-shape), foliate (leaf-shape), and circumvallate (ringed-circle). All papillae except the filiform have taste buds on their surface. Some act directly by ion channels, others act indirectly.
- Fungiform papillae - as the name suggests, are slightly mushroom shaped if looked at in section. These are present mostly at the apex (tip) of the tongue.
- Filiform papillae - these are thin, longer papillae that don't contain taste buds but are the most numerous. These papillae are mechanical and not involved in gustation.
- Foliate papillae - these are ridges and grooves towards the posterior part of the tongue.
- Circumvallate papillae - there are only about 3-14 of these papillae on most people, and they are present at the back of the oral part of the tongue. They are arranged in a circular-shaped row just in front of the sulcus terminalis of the tongue.
Clich and see a short video on the tounge."Taste Buds Video"
Structure of Taste Buds
Each taste bud is flask-like in shape, its broad base resting on the corium, and its neck opening by an orifice, the gustatory pore, between the cells of the epithelium.
The bud is formed by two kinds of cells: supporting cells and gustatory cells.
The supporting cells are mostly arranged like the staves of a cask, and form an outer envelope for the bud. Some, however, are found in the interior of the bud between the gustatory cells. The gustatory cells occupy the central portion of the bud; they are spindle-shaped, and each possesses a large spherical nucleus near the middle of the cell. The peripheral end of the cell terminates at the gustatory pore in a fine hair-like filament, the gustatory hair.
The central process passes toward the deep extremity of the bud, and there ends in single or bifurcated varicosities.
The nerve fibrils after losing their medullary sheaths enter the taste bud, and end in fine extremities between the gustatory cells; other nerve fibrils ramify between the supporting cells and terminate in fine extremities; these, however, are believed to be nerves of ordinary sensation and not gustatory.
Types of Taste
- Salt
- Arguably the simplest receptor found in the mouth is the salt (NaCl) receptor. An ion channel in the taste cell wall allows Na+ ions to enter the cell. This on its own depolarizes the cell, and opens voltage-regulated Ca2+ gates, flooding the cell with ions and leading to neurotransmitter release. This sodium channel is known as EnAC and is composed of three subunits. EnAC can be blocked by the drug amiloride in many mammals, especially rats. The sensitivity of the salt taste to amiloride in humans, however, is much less pronounced, leading to conjecture that there may be additional receptor proteins besides EnAC that may not have been discovered yet.
- Sour
- Sour taste signals the presence of acidic compounds (H+ ions in solution). There are three different receptor proteins at work in sour taste. The first is a simple ion channel which allows hydrogen ions to flow directly into the cell. The protein for this is EnAC, the same protein involved in the distinction of salt taste (this implies a relationship between salt and sour receptors and could explain why salty taste is reduced when a sour taste is present). There are also H+ gated channels present. The first is a K+ channel, which ordinarily allows K+ ions to escape from the cell. H+ ions block these, trapping the potassium ions inside the cell (this receptor is classified as MDEG1 of the EnAC/Deg Family). A third protein opens to Na+ ions when a hydrogen ion attaches to it, allowing the sodium ions to flow down the concentration gradient into the cell. The influx of ions leads to the opening of a voltage regulated Ca2+ gate. These receptors work together and lead to depolarization of the cell and neurotransmitter release.
- Bitter
- There are many classes of bitter compounds which can be chemically very different. It is interesting that the human body has evolved a very sophisticated sense for bitter substances: we can distinguish between the many radically different compounds which produce a generally “bitter” response. This may be because the sense of bitter taste is so important to survival, as ingesting a bitter compound may lead to injury or death. Bitter compounds act through structures in the taste cell walls called G-protein coupled receptors (GPCR’s). Recently, a new group of GPCR’s was discovered, known as the T2R’s, which it is thought respond to only bitter stimuli. When the bitter compound activates the GPCR, it in turn releases gustducin, the G-protein it was coupled to. Gustducin is made of three subunits. When it is activated by the GPCR, its subunits break apart and activate phosphodiesterase, a nearby enzyme, which in turn converts a precursor within the cell into a secondary messenger, which closes potassium ion channels. As well, this secondary messenger can stimulate the endoplasmic reticulum to release Ca2+, which contributes to depolarization. This leads to a build-up of potassium ions in the cell, depolarization, and neurotransmitter release. It is also possible for some bitter tastants to interact directly with the G-protein, because of a structural similarity to the relevant GPCR.
- Sweet
- Like bitter tastes, sweet taste transduction involves GPCR’s. The specific mechanism depends on the specific molecule. “Natural” sweeteners such as saccharides activate the GPCR, which releases gustducin. The gustducin then activates the molecule adenylate cyclase, which is already inside the cell. This molecule increases concentration of the molecule cAMP, or adenosine 3', 5'-cyclic monophosphate. This protein will either directly or indirectly close potassium ion channels, leading to depolarization and neurotransmitter release. Synthetic sweeteners such as saccharin activate different GPCR’s, initiating a similar process of protein transitions, starting with the protein phospholipase A, which ultimately leads to the blocking of potassium ion channels.
- Umami
- It is thought that umami receptors act much the same way as bitter and sweet receptors (they involve GPCR’s), but not much is known about their specific function. It is thought that the amino acid L-glutamate bonds to a type of GPCR known as a metabotropic glutamate receptor (mGluR4). This causes the G-protein complex to activate a secondary receptor, which ultimately leads to neurotransmitter release. The intermediate steps are not known.
Disorders of the Tongue
- A range of tongue disorders
- Loss of taste
- You may lose your sense of taste if the facial nerve is damaged. Then there is also Sjogren's Syndrome where the saliva production is reduced. In most cases the loss of taste is typically a symptom of anosmia - a loss of the sense of smell.
- Sore tongue
- It is usually caused by some form of trauma, such as biting your tongue, or eating piping-hot or highly acidic food or drink.
- If your top and bottom teeth don’t fit neatly together, tongue trauma is more likely.
- Some people may experience a sore tongue from grinding their teeth (bruxism).
- Disorders such as diabetes, aneamia, some types of vitamin deficiency and certain skin diseases can include a sore tongue among the range of symptoms.
- Black hairy tongue
- While the term ‘black hairy tongue’ suggests the tongue surface looks black, it may also be dark yellow, brown, green or white. The tongue papillae are constantly renewing themselves and, usually, the old cells are shed as the new cells emerge. Black hairy tongue, a comparatively rare condition, is caused by the failure of the old cells to shed. The overgrowth of papillae trap food and bacteria, which create the characteristic dark ‘coat’ on the tongue’s surface, while the tongue looks furred because of the layering of unshed papillae. The cause isn’t known.
- Risk factors include:
- Poor oral hygiene
- Cigarette smoking
- Particular antibiotics
- Chemotherapy and radiation treatment for cancers of the head and neck
- Poorly managed diabetes.
- Glossodynia
- A condition characterised by a burning sensation on the tongue.
- Benign migratory glossitis
- This condition is characterised by irregular and inflamed patches on the tongue surface that often have white borders. The tongue may be generally swollen, red and sore. Another name for this condition is geographic tongue. The cause of benign migratory glossitis is unknown.
- Risk factors are thought to include:
- Mineral or vitamin deficiencies
- Local irritants, such as strong mouthwashes, cigarettes or alcohol
- Certain forms of anaemia
- Infection
- Certain medications
- Stress
- Tongue-tie
- Ankyloglossia, commonly known as 'tongue tie'.
- Is a congenital oral anomaly which may decrease mobility of the tongue tip and is caused by a short, thick frenulum. Ankyloglossia varies in degree of severity from mild cases characterized by mucous membrane bands to complete ankyloglossia whereby the tongue is tethered to the floor of the mouth.
Olfactory System
In humans the sence of Smell is received in nasopharynx. Airborne molecules go into solution on moist epithelial surface of nasal passage. An olfactory receptors neuron sends an impulse via Cranial nerve I the olfactory nerve.
Receptors
Humans have 347 functional odor receptor genes; the other genes have nonsense mutations. This number was determined by analyzing the genome in the Human Genome Project; the number may vary among ethnic groups, and does vary among individuals. For example, not all people can smell androstenone, a component of male sweat.
Each olfactory receptor neuron in the nose expresses only one functional odor receptor. Odor receptor nerve cells may function like a key-lock system: if the odor molecules can fit into the lock the nerve cell will respond. According to shape theory, each receptor detects a feature of the odor molecule. Weak-shape theory, known as odotope theory, suggests that different receptors detect only small pieces of molecules, and these minimal inputs are combined to create a larger olfactory perception (similar to the way visual perception is built up of smaller, information-poor sensations, combined and refined to create a detailed overall perception). An alternative theory, the vibration theory proposed by Luca Turin (1996, 2002), posits that odor receptors detect the frequencies of vibrations of odor molecules in the infrared range by electron tunnelling. However, the behavioral predictions of this theory have been found lacking (Keller and Vosshall, 2004).
An olfactory receptor neuron, also called an olfactory sensory neuron, is the primary transduction cell in the olfactory system. Humans have about 40 million olfactory receptor neurons. In verebrates, olfactory receptor neurons reside on the olfactory epithelium in the nasal cavity. These cells are bipolar neurons with a dendrite facing the interior space of the nasal cavity and an axon that travels along the olfactory nerve to the olfactory bulb.
Many tiny hair-like cilia protrude from the olfactory receptor cell's dendrite into the mucus covering the surface of the olfactory epithelium. These cillia contain olfactory receptors, a type of G protein-coupled receptor. Each olfactory receptor cell contains only one type of olfactory receptor, but many separate olfactory receptor cells contain the same type of olfactory receptor. The axons of olfactory receptor cells of the same type converge to form glomeruli in the olfactory bulb.
Olfactory receptors can bind to a variety of odor molecules. The activated olfactory receptor in turn activates the intracellular G-protein GOLF, and adenylate cyclase and production of Cyclic AMP opens ion channels in the cell membrane, resulting in an influx of sodium and calcium ions into the cell. This influx of positive ions causes the neuron to depolarize, generating an action potential.
Individual olfactory receptor neurons are replaced approximately every 40 days by neural stem cells residing in the olfactory epithelium. The regeneration of olfactory receptor cells, as one of the only few instances of adult neurogenesis in the central nervous system, has raised considerable interest in dissecting the pathways for neural development and differentiation in adult organisms.
In the brain
The axons from all the thousands of cells expressing the same odor receptor converge in the olfactory bulb. Mitral cells in the olfactory bulb send the information about the individual features to other parts of the olfactory system in the brain, which puts together the features into a representation of the odor. Since most odor molecules have many individual features, the combination of features gives the olfactory system a broad range of odors that it can detect.
Odor information is easily stored in long term memory and has strong connections to emotional memory. This is possibly due to the olfactory system's close anatomical ties to the limbic system and hippocampus, areas of the brain that have long been known to be involved in emotion and place memory, respectively.
Pheromonal olfaction
Some pheromones are detected by the olfactory system, although in many vertebrates pheromones are also detected by the vomeronasal organ, located in the vomer, between the nose and the mouth. Snakes use it to smell prey, sticking their tongue out and touching it to the organ. Some mammals make a face called flehmen to direct air to this organ. In humans, it is unknown whether or not pheromones exist.
Olfaction and Gustation
Olfaction, taste and trigeminal receptors together contribute to flavor. It should be emphasized that there are no more than 5 distinctive tastes: salty, sour, sweet, bitter, and umami. The 10,000 different scents which humans usually recognize as 'tastes' are often lost or severely diminished with the loss of olfaction. This is the reason why food has little flavor when your nose is blocked, as from a cold.
Disorders of Olfaction
Anosmia:is the lack of olfaction, or a loss of the sense of smell. It can be either temporary or permanent. A related term, hyposmia refers to a decrease in the ability to smell. Some people may be anosmic for one particular odor. This is called "specific anosmia" and may be genetically based. Anosmia can be diagnosed by doctors by using scratch-n-sniff odor tests or by using commonly available odors such as coffee, lemon, and cinnamon.
While termed as a disability, anosmia is often viewed in the medical field as a trivial problem. This is not always the case - esthesioneuroblastoma is a cancerous tumor originating in or near the olfactory nerve. This is a serious condition - if you suspect that you have lost your sense of smell, see an Otolaryngologist (Ear, Nose and Throat doctor) immediately.
Anosmia can have a number of detrimental effects. Patients with anosmia may find food less appetizing. Loss of smell can also be dangerous because it hinders the detection of gas leaks, fire, body odor, and spoiled food. The common view of anosmia as trivial can make it more difficult for a patient to receive the same types of medical aid as someone who has lost other senses, such as hearing or sight.
Losing an established and sentimental smell memory (e.g. the smell of grass, of a grandparent's attic, of a particular book, of loved ones, or of oneself) has been known to cause feelings of depression.
Loss of olfaction may lead to the loss of libido, even to the point of impotency.
A temporary loss of smell can be caused by a stuffy nose or infection. In contrast, a permanent loss of smell may be caused by death of olfactory receptor neurons in the nose, or by brain injury in which there is damage to the olfactory nerve or damage to brain areas that process smell. The lack of the sense of smell at birth, usually due to genetic factors, is referred as congenital anosmia. Anosmia may be an early sign of degenerative brain diseases such as Parkinson's disease and Alzheimer's disease. Another specific cause of permanent loss could be from damage to olfactory receptor neurons due to use of nasal sprays. To avoid loss of smell from nasal spays, use them for only a short amount of time. Nasal sprays that are used to treat allergy related congestion are the only nasal sprays that are safe to use for extended periods of time. Esthesioneuroblastomais an exeedingly rare cancerous tumor that originates in or near the olfactory nerve.
- Hyposmia
- Decreased ability to smell
- Phantosmia
- Phantosmia is the phenomenon of smelling odors that aren't really present. (AKA Phantom odors) The most common odors are unpleasent smells such as rotting flesh, vomit, feces, smoke etc. Phantosmia often results from damage to the nervous tissue in the olfactory system. The damage can be caused by viral infection, trauma, surgery, and possibly exposure to toxins or drugs. It can also be induced by epilepsy affecting the olfactory cortex. It is also thought the condition can have psychiatric origins.
- Dysosmia
- Things do smell differently than they should.
The Sense of Vision
Vision needs to have the work of both the eyes and the brain to process any information. The majority of the stimuli is done in the eyes and then the information is sent to the brain by the way of nerve impulses. Atleast one-third of the information of what the eye sees is processed in the cerebral cortex of the brain.
Anatomy of the Eye
The human eye is a elongated ball about 1-inch (2.5 cm) in diameter and is protected by a bony socket in the skull. The eye has three layers or coats that make up the exterior wall of the eyeball, which are the sclera, choroid, and retina.
- Sclera
- The outer layer of the eye is the sclera, which is a tough white fibrous layer that maintains, protects and supports the shape of the eye. The front of the sclera is transparent and is called the cornea. The cornea refracts light rays and acts like the outer window of the eye.
- Choroid
- The middle thin layer of the eye is the choroid, also known as the choroidea or choroid coat, it is the vascular layer of the eye lying between the retina and the sclera. The choroid provides oxygen and nourishment to the outer layers of the retina. It also contains a nonreflective pigment that acts as a light shield and prevents light from scattering. Light enters the front of the eye throught a hole in the choroid coat called the pupil. The iris contracts and dilates to compensate for the changes in light intensity. If the light is bright the iris then contracts making the puple smaller, and if the light is dim, the iris diliates making the pupil bigger. Just posterior to the iris is the lens, which is composed mainly of proteins called crystallins. The lens is attached by the zonules to the ciliary body that contains the ciliary muscles that control the shape of the lens for accommodation. Along with the ciliary body and iris, the choroid forms the uveal tract. The uvea is the middle of the three concentric layers that make up an eye. The name is possibly a reference to its almost black color, wrinkled appearance and grape-like size and shape when stripped intact from a cadaveric eye.
- Retina
- The third or the innermost layer of the eye is call the retina. In adult humans the entire retina is 72% of a sphere about 22 mm in diameter. The retina lays over the back two thirds of the choroid coat, which is located in the posterior compartment. The compartment is filled with vitreous humor which is a clear, gelatinous material. Within the retina there are cells called rod cells and cone cells also known as photoreceptors. The rod cells are very senstive to light and do not see color, that is why that when we are in a darkend room we see only shades of gray. The cone cells are sensitive to different wavelengths of light, and that is how we are able to tell different colors. It is a lack of cones sensitive to red, blue, or green light that causes individuals to have deficiencies in color vision or various kinds of color blindness. At the center of the retina is the optic disc, sometimes known as "the blind spot" because it lacks photoreceptors. It is where the optic nerve leaves the eye and takes the nerve impulses to the brain. The cornea and the lens of the eye focuses the light onto a small area of the retina called the fovea centralis where the cone cells are densely packed. The fovea is a pit that has the highest visual acuity and is responsible for our sharp central vision - there are no rods in the fovea.
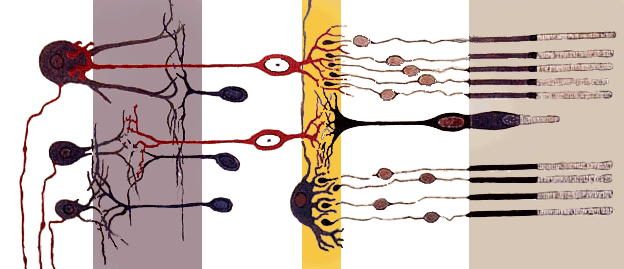
Retina's simplified axial organisation. The retina is a stack of several neuronal layers. Light is concentrated from the eye and passes across these layers (from left to right) to hit the photoreceptors (right layer). This elicits chemical transformation mediating a propagation of signal to the bipolar and horizontal cells (middle yellow layer). The signal is then propagated to the amacrine and ganglion cells. These neurons ultimately may produce action potentials on their axons. This spatiotemporal pattern of spikes determines the raw input from the eyes to the brain.
- Photoreceptors
- A photoreceptor, or photoreceptor cell, is a specialized type of neuron found in the eye's retina that is capable of phototransduction. More specifically, the photoreceptor sends signals to other neurons by a change in its membrane potential when it absorbs photons. Eventually, this information will be used by the visual system to form a complete representation of the visual world. There are 2 types of photoreceptors: rods are responsible for scotopic, or night vision, whereas cones are responsible for photopic, or daytime vision as well as color perception.
- Extraocular muscles
- Each eye has six muscles that control its movements: the lateral rectus, the medial rectus, the inferior rectus, the superior rectus, the inferior oblique, and the superior oblique. When the muscles exert different tensions, a torque is exerted on the globe that causes it to turn. This is an almost pure rotation, with only about one millimeter of translation, thus, the eye can be considered as undergoing rotations about a single point in the center of the eye. Five of the extraocular muscles have their origin in the back of the orbit in a fibrous ring called the annulus of Zinn. Four of these then course forward through the orbit and insert onto the globe on its anterior half (i.e., in front of the eye's equator). These muscles are named after their straight paths, and are called the four rectus muscles, or four recti. They insert on the globe at 12, 3, 6, and 9 o'clock, and are called the superior, lateral, inferior and medial rectus muscles. (Note that lateral and medial are relative to the subject, with lateral toward the side and medial toward the midline, thus the medial rectus is the muscle closest to the nose).
Eye Movement
The visual system in the brain is too slow to process that information if the images are slipping across the retina at more than a few degrees per second, thus, for humans to be able to see while moving, the brain must compensate for the motion of the head by turning the eyes. To get a clear view of the world, the brain must turn the eyes so that the image of the object of regard falls on the fovea. Eye movements are thus very important for visual perception, and any failure to make them correctly can lead to serious visual disabilities. Having two eyes is an added complication, because the brain must point both of them accurately enough that the object of regard falls on corresponding points of the two retinas; otherwise, double vision would occur. The movements of different body parts are controlled by striated muscles acting around joints. The movements of the eye are no exception, but they have special advantages not shared by skeletal muscles and joints, and so are considerably different.
- Try This Experiment
- Hold your hand up, about one foot (30 cm) in front of your nose. Keep your head still, and shake your hand from side to side, slowly at first, and then faster and faster. At first you will be able to see your fingers quite clearly. But as the frequency of shaking passes about one hertz, the fingers will become a blur. Now, keep your hand still, and shake your head (up and down or left and right). No matter how fast you shake your head, the image of your fingers remains clear. This demonstrates that the brain can move the eyes opposite to head motion much better than it can follow, or pursue, a hand movement. When your pursuit system fails to keep up with the moving hand, images slip on the retina and you see a blurred hand.
How we see an object
- The light rays enter the eye through the cornea (transparent front portion of eye to focus the light rays)
- Then, light rays move through the pupil, which is surrounded by Iris to keep out extra light
- Then, light rays move through the crystalline lens (Clear lens to further focus the light rays )
- Then, light rays move through the vitreous humor (clear jelly like substance)
- Then, light rays fall on the retina, which processes and converts incident light to neuron signals using special pigments in rod and cone cells.
- These neuron signals are transmitted through the optic nerve,
- Then, the neuron signals move through the visual pathway - Optic nerve > Optic Chiasm > Optic Tract > Optic Radiations > Cortex
- Then, the neuron signals reach the occipital (visual) cortex and its radiations for the brain's processing.
- The visual cortex interprets the signals as images and along with other parts of the brain, interpret the images to extract form, meaning, memory and context of the images.
Depth Perception
Depth perception is the visual ability to perceive the world in three dimensions. It is a trait common to many higher animals. Depth perception allows the beholder to accurately gauge the distance to an object.
Depth perception is often confused with binocular vision, also known as Stereopsis. Depth perception does rely on binocular vision, but it also uses many other monocular cues.
Diseases, disorders, and age-related changes
There are many diseases, disorders, and age-related changes that may affect the eyes and surrounding structures. As the eye ages certain changes occur that can be attributed solely to the aging process. Most of these anatomic and physiologic processes follow a gradual decline. With aging, the quality of vision worsens due to reasons independent of aging eye diseases. While there are many changes of significance in the nondiseased eye, the most functionally important changes seem to be a reduction in pupil size and the loss of accommodation or focusing capability (presbyopia). The area of the pupil governs the amount of light that can reach the retina. The extent to which the pupil dilates also decreases with age. Because of the smaller pupil size, older eyes receive much less light at the retina. In comparison to younger people, it is as though older persons wear medium-density sunglasses in bright light and extremely dark glasses in dim light. Therefore, for any detailed visually guided tasks on which performance varies with illumination, older persons require extra lighting.
- Color Blindness
- Color Blindness or color vision deficiency, in humans is the inability to perceive differences between some or all colors that other people can distinguish. It is most often of genetic nature, but may also occur because of eye, nerve, or brain damage, or due to exposure to certain chemicals. There are many types of color blindness. The most common variety are hereditary (genetic) photoreceptor disorders, but it is also possible to acquire color blindness through damage to the retina, optic nerve, or higher brain areas. There is generally no treatment to cure color deficiencies, however, certain types of tinted filters and contact lenses may help an individual to distinguish different colors better.
- Night Blindnes
- Also known as Nyctalopia, is a condition making it difficult or impossible to see in the dark. It is a symptom of several eye diseases. Night blindness may exist from birth, or be caused by injury or malnutrition (for example, a lack of vitamin A). The most common cause of nyctalopia is retinitis pigmentosa, a disorder in which the rod cells in the retina gradually lose their ability to respond to the light. Patients suffering from this genetic condition have progressive nyctalopia and eventually their day-time vision may also be affected. In congenital stationary night blindness the rods do not work from birth, but as the name implies, sufferers do not get worse. Another cause of night blindness is a deficiency of retinol, or vitamin A, found in fish oils, liver and dairy products.
- Day Blindness
- Also known as Hemeralopia is the inability to see clearly in bright light. The daytime vision gets worse and worse. Nighttime vision remains unchanged due to the use of rods as opposed to cones (during the day), which get affected by hemeralopia and in turn degrade the daytime optical response.
- Cataract
- A cataract is an opacity which develops in the crystalline lens of the eye or in its envelope. Cataracts typically progress slowly to cause vision loss and are potentially blinding if left untreated. Cataracts form for a variety of reasons, including long-term ultraviolet exposure, secondary effects of diseases such as diabetes, or simply due to advanced age; they are usually a result of denaturation of lens proteins. Genetic factors are often a cause of congenital cataracts and may also play a role in predisposing someone to cataracts. Half of all people between the ages of 65 and 74 and about 70% of those over 75 have some cataract formation. Cataracts may also be produced by eye injury or physical trauma.
- Floater
- Also known as "Muscae Volitantes" are deposits of various size, shape, consistency, refractive index, and motility within the eye's normally transparent vitreous humour. Floaters are suspended in the vitreous humour, the thick fluid or gel that fills the eye. Thus, they generally follow the rapid motions of the eye, while drifting slowly within the fluid. Floaters located slightly to the side of one's direction of gaze can be particularly annoying. When they are first noticed, the natural reaction is to attempt to look directly at them. However, attempting to shift one's gaze toward them can be difficult since floaters follow the motion of the eye, remaining to the side of the direction of gaze. Floaters are, in fact, visible only because they do not remain perfectly fixed within the eye. Floaters are particularly noticeable when lying on one's back and gazing at blue sky. Despite the name "floaters", many of these specks have a tendency to sink toward the bottom of the eyeball, in whichever way the eyeball is oriented; the supine position tends to concentrate them near the fovea, which is the center of gaze, while the textureless and evenly lit sky forms an ideal background against which to view them. Floaters are not uncommon, and do not cause problems for most sufferers. However, floaters are more than a nuisance and a distraction to those with severe cases, especially if the spots seem to constantly drift through the field of vision. The shapes are shadows projected onto the retina by tiny structures of protein or other cell debris discarded over the years and trapped in the vitreous humour. It should also be noted that they can even be seen when the eyes are closed on especially bright days, when sufficient light penetrates the eyelids to cast the shadows. It is not, however, only elderly people who suffer from floaters; they can certainly become a problem to younger people, especially if they are myopic. They are also common after cataract operations or after trauma. In some cases, floaters are congenital. There are various causes for the appearance of floaters, of which the most common are described here. The most common cause of floaters is shrinkage of the vitreous humour: this gel-like substance consists of 99% water and 1% solid elements. The solid portion consists of a network of collagen and hyaluronic acid, with the latter retaining water molecules. Patients with retinal tears may experience floaters if red blood cells are released from leaky blood vessels, and those with a posterior uveitis or vitritis, as in toxoplasmosis, may experience multiple floaters and decreased vision due to the accummulation of white blood cells in the vitreous humour.
- Glaucoma
- A group of diseases of the optic nerve involving loss of retinal ganglion cells in a characteristic pattern of optic neuropathy. Although raised intraocular pressure is a significant risk factor for developing glaucoma, there is no set threshold for intraocular pressure that causes glaucoma. One person may develop nerve damage at a relatively low pressure, while another person may have high eye pressures for years and yet never develop damage. Untreated glaucoma leads to permanent damage of the optic nerve and resultant visual field loss, which can progress to blindness.
- Visual Agnosia
Visual agnosia is the inability of the brain to make sense of or make use of some part of otherwise normal visual stimulus, and is typified by the inability to recognize familiar objects or faces. This is distinct from blindness, which is a lack of sensory input to the brain due to damage to the eye or optic nerve. Visual agnosia is often due to damage, such as stroke, in posterior parietal lobe in the right hemisphere of the brain.
The specific symptoms can vary depending on the cause of the agnosia. Some sufferers are unable to copy drawings, but are able to manipulate objects with good dexterity.Commonly patients can describe objects in their visual field in great detail, including such aspects as color, texture, and shape, but are unable to recognize them. Similarly, patients can often describe familiar objects from memory despite their visual problems
Careful analysis of the nature of visual agnosia has led to improved understanding of the brain's role in normal vision.
The Senses Of Hearing
The ear is the sense organ that detects sound and plays a major role in the sense of balance and body position. The sensory receptors for both hearing and equilibrium are to be found in the inner ear consisting of hair cells that have stereocilia (long mircovilli). The stereocillia are extremely sensitive to mechanical stimulations, which are known as mechanoreceptors.
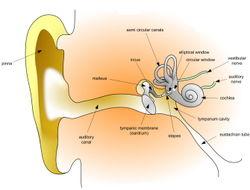
Anatomy of the Ear
The ear has three divisions: the outer ear, middle ear, and the inner ear.
- Outer Ear (Auricle, Ear Canal, Surface of Ear Drum)
- The outer ear is the most external portion of the ear. The outer ear includes the pinna (also called auricle), the ear canal, and the very most superficial layer of the ear drum (also called the tympanic membrane). Although the word "ear" may properly refer to the pinna (the flesh covered cartilage appendage on either side of the head), this portion of the ear is not vital for hearing. The complicated design of the human outer ear does help capture sound, but the most important functional aspect of the human outer ear is the ear canal itself. This outer ear canal skin is applied to cartilage; the thinner skin of the deep canal lies on the bone of the skull. If the ear canal is not open, hearing will be dampened. Ear wax (medical name - cerumen) is produced by glands in the skin of the outer portion of the ear canal. Only the thicker cerumen-producing ear canal skin has hairs. The outer ear ends at the most superficial layer of the tympanic membrane. The tympanic membrane is commonly called the ear drum.
- Middle Ear (Air Filled Cavity behind the Ear Drum, includes most of the Ear Drum, and Ear Bones)
- The middle ear includes most of the ear drum (tympanic membrane) and the 3 ear bones ossicles: malleus (or hammer), incus (or anvil), and stapes (or stirrup). The opening of the Eustachian tube is also within the middle ear. The malleus has a long process (the handle) that is attached to the mobile portion of the ear drum. The incus is the bridge between the malleus and stapes. The stapes is the smallest named bone in the human body. The stapes transfers the vibrations of the incus to the oval window, a portion of the inner ear to which it is connected. It is the final bone in the chain to transfer vibrations from the eardrum to the inner ear. The arrangement of these 3 bones is a sort of Rube Goldberg device: movement of the tympanic membrane causes movement of the first bone, which causes movement of the second, which causes movement of the third. When this third bone pushes down, it causes movement of fluid within the cochlea (a portion of the inner ear). This particular fluid only moves when the stapes footplate is depressed into the inner ear. Unlike the open ear canal, however, the air of the middle ear is not in direct contact with the atmosphere outside the body. The Eustachian tube connects from the chamber of the middle ear to the back of the pharynx. The middle ear in humans is very much like a specialized paranasal sinus, called the tympanic cavity, it, like the paranasal sinuses, is a hollow mucosa lined cavity in the skull that is ventilated through the nose. The mastoid portion of the temporal bone, which can be felt as a bump in the skull behind the pinna, also contains air, which ventilates through the middle ear.
- Inner Ear (Cochlea, Vestibule, and Semi-Circular Canals)
- The inner ear includes both the organ of hearing (the cochlea) and a sense organ that is attuned to the effects of both gravity and motion labyrinth or vestibular apparatus. The balance portion of the inner ear consists of three semi-circular canals and the vestibule. The inner ear is encased in the hardest bone of the body. Within this ivory hard bone, there are fluid-filled hollows. Within the cochlea are three fluid filled spaces: the tympanic canal, the vestibular canal, and the middle canal. The eighth cranial nerve comes from the brain stem to enter the inner ear. When sound strikes the ear drum, the movement is transferred to the footplate of the stapes, which presses into one of the fluid-filled ducts of the cochlea. The hair cells in the organ of Corti are tuned to certain sound frequencies, being responsive to high frequencies near the oval window and to low frequencies near the apex of the cochlea.
- The fluid inside this duct is moved, flowing against the receptor cells of the organ of Corti, which fire. These stimulate the Spiral Ganglion, which sends information through the auditory portion of the eighth cranial nerve to the brain.
- Hair Cell
- Hair cells are columnar cells, each with a bundle of 100-200 specialized cilia at the top, for which they are named. These cillia are the mechanosensors for hearing. Lightly resting atop the longest cilia is the tectorial membrane, which moves back and forth with each cycle of sound, tilting the cilia and allowing electric current into the hair cell. Hair cells, like the photoreceptors of the eye, show a graded response, instead of the spikes typical of other neurons. These graded potentials are not bound by the “all or none” properties of an action potential. One may ask how such a wiggle of a hair bundle triggers a difference in membrane potential. The current model is that cilia are attached to one another by “tip links”, structures which link the tips of one cilium to another. Stretching and compressing the tip links may open an ion channel and produce the receptor potential in the hair cell. There are far fewer hair cells than afferent nerve fibers in the cochlea. The nerve that innervates the cochlea is the vestibulocochlear nerve, or cranial nerve number VIII. Neuronal dendrites innervate cochlear hair cells. The neurotransmitter itself is thought to be glutamate. At the presynaptic juncture, there is a distinct “presynaptic dense body” or ribbon. This dense body is surrounded by synaptic vesicles and is thought to aid in the fast release of neurotransmitter. Efferent projections from the brain to the cochlea also play a role in the perception of sound. Efferent synapses occur on outer hair cells and on afferent dendrites under inner hair cells.
Process of Hearing
Detection of sound motion is associated with the right posterior superior temporal gyrus. The superior temporal gyrus contains several important structures of the brain, including: (1)marking the location of the primary auditory cortex, the cortical region responsible for the sensation of sound. Sections 41 and 42 are called the primary auditory area of the cerebrum, and processes the basic characteristics of sound such as pitch and rythym. The auditory association area is located within the temporal lobe of the brain, in an area called the Wernicke's area, or area 22. This area, near the lateral cerebral sulcus, is an important region for the processing of acoustic energy so that it can be distinguished as speech, music, or noise. It also interprets words that are heard into an associated thought pattern of understanding. The gnostic area of the cerebum, (areas 5, 7, 39 and 40) helps to integrate all incomming sense patterns so that a common thought can be formed (correlated) using all arriving sensory information.
Hearing Under Water
Hearing threshold and the ability to localize sound sources are reduced underwater. in which the speed of sound is faster than in air. Underwater, hearing is by bone conduction and localization of sound appears to depend on differences in amplitude detected by bone conduction.
Localization of Sound by Humans
Humans are normally able to hear a variety of sound frequencies, from about 20Hz to 20kHz. Our ability to estimate just where the sound is coming from, sound localization, is dependant on both hearing ability of each of the two ears, and the exact quality of the sound. Since each ear lies on an opposite side of the head, a sound will reach the closest ear first, and its amplitide will be loudest in that ear. Much of the brain's ability to localize sound depends on interaural (between ears) intensity differences and interaural temporal or phase differences.
Two mechanisms are known to be used.
Bushy neurons can resolve time differences as small as the time it takes sound to pass one ear and reach the other (10 milliseconds). For high frequencies, frequencies with a wavelength shorter than the listener's head, more sound reaches the nearer ear. Human echolocation is a technique involving echolocation used by some blind humans to navigate within their environment.
Process of Equilibrium
Equilibrioception or sense of balance is one of the physiological senses. It allows humans and animals to walk without falling. Some animals are better in this than humans, for example allowing a cat (as a quadruped using its inner ear and tail) to walk on a thin fence. All forms of equilibrioception can be described as the detection of acceleration.
It is determined by the level of fluid properly called endolymph in the labyrinth - a complex set of tubing in the inner ear.
When the sense of balance is interrupted it causes dizziness, disorientation and nausea.
You can temporarily disturb your sense of balance by closing your eyes and turning rapidly in circles five or six times. This starts the fluid swirling in circles inside your ear canal. When you stop turning it takes a few seconds for the fluid to lose momentum, and until then the sense from your inner ear conflicts with the information coming from your vision, causing dizziness and disorientation. Most astronauts find that their sense of balance is impaired when in orbit, because there is not enough gravity to keep the ear's fluid in balance. This causes a form of motion sickness called space sickness.
Disorders with the Ear
- Deafness
- The word deaf can have at least two different meanings. The first term is used to indicate the presence of enough hearing loss such that an individual is not sensitive to sound. Someone with a partial loss of hearing is more likely to be referred to as hearing impaired or the qualified partially deaf. The second term is used to indicate someone who was born without the sense of hearing or total deafness.
- Otitis Media
- An inflammation of the middle ear segment. It is usually associated with a buildup of fluid and frequently causes an earache. The fluid may or may not be infected. The typical progress of otitis media is: the tissues surrounding the Eustachian tube swell due to an infection and/or severe congestion. The Eustachian tube remains blocked most of the time. The air present in the middle ear is slowly absorbed into the surrounding tissues. A strong negative pressure creates a vacuum in the middle ear. The vacuum reaches a point where fluid from the surrounding tissues accumulates in the middle ear. Streptococcus pneumoniae and Haemophilus influenzae are the most common bacterial causes of otitis media. As well as being caused by Streptococcus pneumoniae and Haemophilus influenzae it can also be caused by the common cold.
- Vertigo (dizziness)
- Vertigo, sometimes called a headrush, is a major symptom of a balance disorder. It is the sensation of spinning while the body is stationary with respect to the earth or surroundings. With the eyes shut, there will be a sensation that the body is in movement, called subjective vertigo; if the eyes are open, the surroundings will appear to move past the field of vision, called objective vertigo. The effects may be slight. It may cause nausea or, if severe, may give rise to difficulty with standing and walking. Vertigo is usually associated with a problem in the inner ear balance mechanisms (vestibular system), in the brain, or with the nerve connections between these two organs. The most common cause is benign paroxysmal positional vertigo, or BPPV. Vertigo can be a symptom of an underlying harmless cause, such as in BPPV or it can suggest more serious problems. These include drug toxicities, strokes or tumors (though these are much less common than BPPV).
- Motion sickness
- Motion sickness is a condition in which the endolymph (the fluid found in the semicircular canals of the inner ears) becomes 'stirred up', causing confusion between the difference between apparent perceived movement (none or very little), and actual movement. Depending on the cause, it is also referred to as seasickness, carsickness, airsickness, or spacesickness. Nausea is the most common symptom of motion sickness. If the motion causing nausea is not resolved, the sufferer will frequently vomit within twenty minutes. Unlike ordinary sickness, vomiting in motion sickness tends not to relieve the nausea.
- Dysacusis
- Dysacusis is a hearing impairment characterized by difficulty in processing details of sound, but not primarily a loss of the ability to perceive sound. May also refer to pain or discomfort due to sound.
- Meniere's Disease
Microtia (meaning 'small ear') is a congenital deformity of the pinna (outer ear). It can be unilateral (one side only) or bilateral (affecting both sides). It occurs in 1 out of about 8,000-10,000 births. In unilateral microtia, the right ear is most typically affected. There are four grades of microtia [1]:
Grade I: A slightly small ear with identifiable structures and a small but present external ear canal Grade II: A partial or hemi-ear with a closed off or stenotic external ear canal producing a conductive hearing loss Grade III: Absence of the external ear with a small peanut vestige structure and an absence of the external ear canal and ear drum Grade IV: Absence of the total ear or anotia. Grade III is most common, and can be corrected by surgery. Typically, testing is first done to determine if the inner ear is intact and hearing is normal. If hearing is normal, the next step (if a canal is not visible externally) will be to determine if a canal exists, by MRI. For younger patients, this is done under sedation. Surgery may not necessarily be attempted until at a later age (generally about age 8, when the ear is full adult size). Cosmetic surgery (building a new outer ear) is done first to ensure position in relation to the other side; the patient's own cartilage is used (taken from ribs or elsewhere). Surgery to build a canal and/or canal opening can then proceed.
Touch
- Haptic From the Greek Haphe, means pertaining to the sense of touch. It is the earliest sense to develop in the fetus, and the development of infants.
- Tactition is the sense of pressure perception, generally in the skin. There are a variety of pressure receptors that respond to variations in pressure.
- Thermoception is the sense of heat and the absence of heat (cold), also by the skin and including internal skin passages. The thermoceptors in the skin are quite different from the homeostatic thermoceptors which provide feedback on internal body temperature.
- Nociception is the perception of pain. It can be classified as from one to three senses, depending on the classification method. The three types of pain receptors are cutaneous (skin), somatic (joints and bones) and visceral (body organs). For a considerable time, it was believed that pain was simply the overloading of pressure receptors, but research in the first half of the 20th century indicated that pain is a distinct phenomenon that intertwines with all other senses, including touch.
Mechanoreceptor
A mechanoreceptor is a sensory receptor that responds to mechanical pressure or distortion. There are four main types in the glabrous skin of humans: Pacinian corpuscles, Meissner's corpuscles, Merkel's discs, and Ruffini corpuscles. There are also mechanoreceptors in the hairy skin, and the hair cells in the cochlea are the most sensitive mechanoreceptors in tranducing air pressure waves into sound.
- Meissner's Corpuscle
Meissner's corpuscles (discovered by the anatomist Georg Meissner (1829-1903)) are a type of mechanoreceptor and more specifically, a tactile corpuscle (corpusculum tactus). They are distributed throughout the skin, but concentrated in areas especially sensitive to light touch, such as the fingertips, palms, soles, lips, tongue, face, nipples and the external skin of the male and female genitals. They are primarily located just beneath the epidermis within the dermal papillae.
Meissner's corpuscles are encapsulated unmyelinated nerve endings, which consist of flattened supportive cells arranged as horizontal lamellae surrounded by a connective tissue capsule. A single nerve fiber meanders between the lamellae and throughout the corpuscle. Any physical deformation in the corpuscle will cause an action potential in the nerve. Since they are rapidly adapting or phasic, the action potentials generated quickly decrease and eventually cease. If the stimulus is removed, the corpuscle regains its shape and while doing so (ie: while physically reforming) causes another volley of action potentials to be generated. (This is the reason one stops "feeling" one's clothes.) Because of their superficial location in the dermis, these corpuscles are particularly sensitive to touch and vibrations, but for the same reasons, they are limited in their detection because they can only signal that something is touching the skin. Feelings of deep pressure (from a poke, for instance) are generated from Pacinian corpuscles (the only other type of phasic tactile mechanoreceptor), which are located deeper in the dermis, and some free nerve endings. Also, Meissner's corpuscles do not detect pain; this is signalled exclusively by free nerve endings.
- Pacinian Corpuscles
Pacinian corpuscles detect gross pressure changes and vibrations. Any deformation in the corpuscle causes action potentials to be generated, by opening pressure-sensitive sodium ion channels in the axon membrane. This allows sodium ions to influx in, creating a receptor potential.
These corpuscles are especially susceptible to vibrations, which they can sense even centimeters away (Kandel et al., 2000). Pacinian corpuscles cause action potentials when the skin is rapidly indented but not when the pressure is steady, due to the layers of connective tissue that cover the nerve ending (Kandel et al., 2000). It is thought that they respond to high velocity changes in joint position.
Pacinian corpuscles have a large receptive field on the skin's surface with an especially sensitive center (Kandel et al., 2000). They only sense stimuli that occur within this field.
- Merkels Discs
Merkel nerve endings are mechanoreceptors found in the skin and mucosa of vertebrates that provide touch information to the brain. Each ending consists of a Merkel cell in close apposition with an enlarged nerve terminal. This is sometimes referred to as a Merkel cell-neurite complex, or a Merkel disk receptor. A single afferent nerve fibre branches to innervate up to 90 such endings. They are classified as slowly adapting type I mechanoreceptors.
- Ruffini Corpuscles
Glossary
- Chemoreception
- The physiological response of a sense organ to a chemical stimulus.
- Papilla
- Specialized epithelial cells which are small projections on the top of the tounge.
- Nasopharynx
- Nasal part of the pharynx that lies behind the nose and above the level of the soft palate.
- Anosmia
- The lack of olfaction, or a loss of the sense of smell.
- Phantosmia
- The phenomenon of smelling odors that aren't really present. (AKA Phantom odors)
- Sclera
- The white outer coating of the eye made of tough fibrin connective tissue which gives the eye its shape and helps to protect the delicate inner parts.
- Choroid
- Is the vascular layer of the eye lying between the retina and the sclera. The choroid provides oxygen and nourishment to the outer layers of the retina.
- Retina
- Is a thin layer of neural cells that lines the back of the eyeball of vertebrates and some cephalopods.
- Outer Ear
- The part of the ear visable to externally.
- Pinna
- The auricle of the ear.
- Auditory Canal
- The tube from the auditory meatus or opening of the ear to the tympanic membrane.
- Middle Ear
- The main cavity of the ear; between the eardrum and the inner ear.
- Tympanic Membrane
- Like a tympanum or drum; acting like a drumhead; as, a tympanic membrane. The membrane in the ear that vibrates to sound.
- Oval Window
- Fenestra that has the base of the stapes attached to it.
- Round Window
- Fenestra leading into the cochlea.
- Ossicles
- The there small bones of tympanum of the ear.
- Malleus
- One of the small bones in the tympanum of the ear; the hammer bone.
- Incus
- One of the small bones in the tympanum of the ear; the anvil bone.
- Stapes
- One of the small bones in the tympanum of the ear; the stirrups bone.
- Auditory Tube
- Either of the paired tubes connecting the middle ears to the nasopharynx; equalizes air pressure on the two sides of the eardrum.
- Inner Ear
- Complex systems of interconnecting cavities; concerned hearing and equilibrium.
- Semicircular Canals
- Certain canals of the inner ear.
- Cochlea
- Is concerned with hearing, resembling a shell of a snail.
Content by Wikibooks . Text is available under the terms of the GNU Free Documentation License