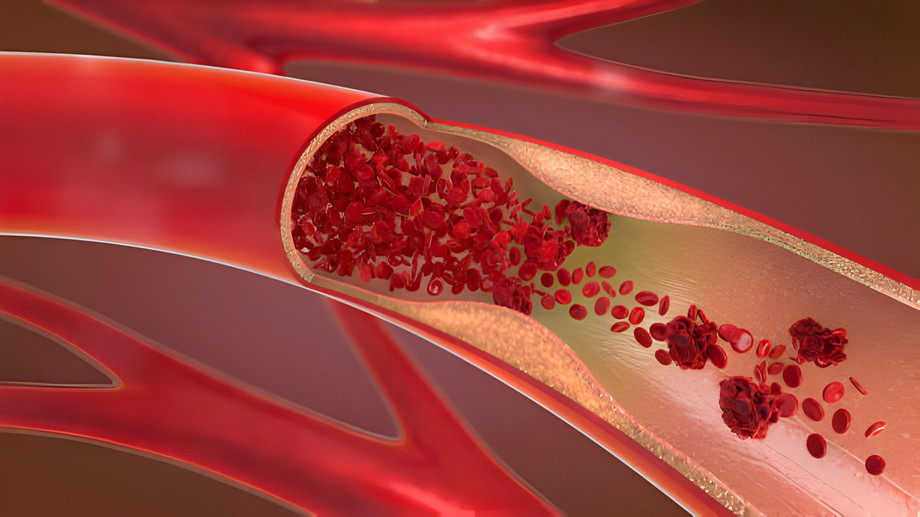
Ischemic heart disease (IHD), a pervasive cardiovascular ailment characterized by reduced blood flow to the heart muscle, continues to pose formidable challenges in clinical management. This article delves into the multifaceted landscape of IHD treatment, exploring a spectrum of therapeutic modalities ranging from pharmacotherapy to revascularization procedures and lifestyle interventions.
Pharmacotherapy: Targeting Underlying Pathophysiology
Pharmacotherapy constitutes the cornerstone of IHD management, aiming to alleviate symptoms, mitigate disease progression, and reduce the risk of adverse cardiovascular events. Medications deployed in the management of IHD encompass a diverse array of agents, including:
-
Antiplatelet Agents: Vital in inhibiting platelet aggregation, agents like aspirin and P2Y12 inhibitors stand as fundamental components in reducing thrombotic events, particularly in acute coronary syndromes (ACS) and post-percutaneous coronary intervention (PCI) settings.
-
Statins: Central to dyslipidemia management, statins exert profound effects in lowering LDL cholesterol levels and mitigating atherosclerosis progression. Beyond lipid-lowering properties, statins exhibit pleiotropic effects, including anti-inflammatory and endothelial function improvement, thus contributing to plaque stabilization and risk reduction.
-
Beta-Blockers: Through modulation of heart rate and blood pressure, beta-blockers play a pivotal role in attenuating myocardial oxygen demand. Particularly beneficial in managing angina symptoms and preventing recurrent myocardial infarction (MI), beta-blockers are indispensable in high-risk cohorts.
-
Calcium Channel Blockers (CCBs): Agents such as amlodipine and verapamil offer vasodilatory effects, ameliorating angina symptoms by dilating coronary arteries and diminishing myocardial oxygen demand. These agents serve as adjuncts in refractory angina or beta-blocker contraindications.
-
Nitrates: Rapid-acting vasodilators like nitroglycerin provide swift relief from angina by promoting coronary artery dilation and reducing preload and afterload. Essential for acute anginal episodes and prophylactic use, nitrates play a pivotal role in symptom management.
-
ACE Inhibitors/ARBs: These agents, pivotal in managing hypertension and heart failure, confer vasodilatory and cardioprotective benefits. By attenuating myocardial remodeling and improving left ventricular function, ACE inhibitors and ARBs hold significance in IHD management.
Revascularization Procedures: Restoring Coronary Perfusion
Revascularization procedures aim to restore coronary blood flow, thereby alleviating ischemia and ameliorating symptoms. The primary modalities include:
-
Percutaneous Coronary Intervention (PCI): Employing catheter-based techniques, PCI encompasses balloon angioplasty and stent placement to optimize coronary patency. It stands as a cornerstone in managing significant coronary stenosis, particularly in acute settings.
-
Coronary Artery Bypass Grafting (CABG): Reserved for complex coronary artery disease and multi-vessel involvement, CABG entails surgical creation of bypass grafts using harvested veins or arteries. It offers a durable solution for reestablishing coronary perfusion in high-risk cohorts.
Lifestyle Interventions: Modifying Risk Factors
Beyond pharmacotherapy and revascularization, lifestyle modifications constitute indispensable pillars in IHD management, addressing modifiable risk factors and fostering cardiovascular health:
-
Smoking Cessation: Essential for reducing cardiovascular risk, smoking cessation interventions aim to curb tobacco use through behavioral counseling and pharmacotherapy, mitigating a major risk factor for IHD.
-
Healthy Diet and Weight Management: Adopting a heart-healthy diet rich in fruits, vegetables, and lean proteins, coupled with weight management strategies, plays a pivotal role in managing dyslipidemia, hypertension, and obesity.
-
Regular Exercise: Regular physical activity enhances cardiovascular fitness, ameliorates blood pressure, and promotes weight loss, thereby mitigating IHD risk factors and improving overall cardiovascular health.
-
Stress Management: Stress reduction techniques, including mindfulness meditation and relaxation therapy, attenuate the impact of psychological stress on cardiovascular health, complementing pharmacotherapy and revascularization strategies.