What is Diabetic Peripheral Neuropathy?
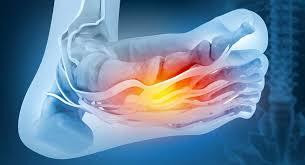
Diabetic peripheral neuropathy, also known as DPN, is a type of nerve damage that affects people with diabetes. It happens when high blood sugar levels damage nerves, especially those in the hands and feet. Over time, this nerve damage causes pain, numbness, tingling and weakness. DPN usually starts in the feet and lower legs before spreading to other parts of the body. It is one of the most common complications of both type 1 and type 2 diabetes.
Symptoms
Some common symptoms of DPN include:
- Numbness, tingling or burning sensations in the feet and lower legs. This is usually described as feeling like pins and needles or walking barefoot on snow.
- Pain in the feet, legs or hands that feels like muscle soreness even at rest. The pain can range from mild to severe.
- Sensitivity to touch. Even light clothing or bedsheets can cause discomfort.
-loss of sensation making it hard to feel things like pain or temperature changes.
- Muscle weakness in the lower legs and feet making it hard to do things like rising on toes.
- Foot problems like blisters and ulcers as loss of sensation prevents feeling injuries.
- Restless legs syndrome where limbs feel uneasy leading to irresistible urge to move them.
- Changes in gait or walking pattern due to loss of sensation in the feet.
The symptoms usually start slowly and worsen over months or years if blood sugar levels remain poorly controlled. Not everyone experiences the same symptoms at the same severity.
Causes of Diabetic Peripheral Neuropathy
High blood glucose levels are the main underlying cause of diabetic nerve damage. Constant exposure to high blood sugar levels makes the peripheral nerves more susceptible to damage over time. Some key factors that increase risk include:
- Duration of diabetes - Longer a person lives with diabetes, higher the chances of developing DPN. Most people develop it after 10-15 years.
- Poor blood sugar control - Higher the A1c or average blood glucose levels, faster the progression of nerve damage. An A1c above 7.0% significantly raises risk.
- Obesity - Being overweight increases insulin resistance and risk of high blood sugar.
- High blood pressure and high cholesterol levels - These contribute to microvascular complications like DPN.
- Genetics - Some people have a genetic predisposition which makes their nerves less tolerant to high glucose levels.
- Age - Risk increases with age as peripheral nerves weaken over time. Older adults are more susceptible.
- Smoking - Smoking constricts blood vessels supplying nerves and worsens diabetic complications.
Diagnosing Diabetic Peripheral Neuropathy
To diagnose DPN, doctors may perform the following tests:
- Medical history and physical exam - Ask about symptoms and check sensation levels with touch.
- Sensory testing - Using tools like tuning forks, cotton balls, pinpricks to check response to vibration, temperature and touch.
- Electromyography (EMG) - A test evaluating speed and effectiveness of nerve signals to detect neuropathy.
- Nerve conduction studies (NCS) - Checks how fast electrical impulses travel through motor and sensory nerves.
- Skin biopsy - Removing a small piece of skin to check epidermal nerve fiber density under microscope.
- Neurological examination - Evaluating muscle strength, reflexes and gait abnormalities.
- Ruling out other causes - Blood tests, MRI etc are done to rule out conditions mimicking neuropathy.
Management of Diabetic Peripheral Neuropathy
Treatment focuses on managing pain, preventing injuries and addressing underlying causes. Some options include:
- Glycemic control - Keeping blood sugar levels as close to normal range helps prevent progression of nerve damage. Insulin therapy and oral medications are used.
- Pain medication - Over-the-counter pain relievers or prescription drugs like gabapentin, pregabalin and duloxetine may ease neuropathic pain.
- Antidepressants - Amitriptyline or nortriptyline help in some cases by altering pain signals.
- Topical treatments - Creams containing lidocaine may temporarily relieve symptoms.
- Supplements - Alpha-lipoic acid supplements showed benefits in some studies.
- Physical therapy - Exercises strengthen leg muscles to prevent injuries from sensory loss.
- Proper foot care - Daily inspection, moisturizing, nail clipping and shoes fitting prevent ulcers and wounds from developing.
- Smoking cessation - If smoker, quitting prevents further nerve damage and speeds up recovery.
With appropriate multidisciplinary management, DPN progression can be slowed down and symptoms managed effectively to maintain quality of life for diabetics. Following treatment plans religiously lowers risk of serious foot complications like amputations arising from nerve-related injuries.
About Author:
Ravina Pandya, Content Writer, has a strong foothold in the market research industry. She specializes in writing well-researched articles from different industries, including food and beverages, information and technology, healthcare, chemical and materials, etc. (https://www.linkedin.com/in/ravina-pandya-1a3984191)
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it