Embedded hardware design plays a critical role in medical technology, where reliability is not just an expectation but a necessity. Designing embedded hardware for life-saving medical devices demands not only technical expertise but also a commitment to safety, precision, and quality. Given the high stakes, from life-support systems to diagnostic equipment, embedded systems in the medical field must operate flawlessly under various conditions. This blog will explore the key considerations in designing reliable embedded hardware design for medical devices, emphasizing the specific standards, technologies, and approaches required to create devices that healthcare professionals and patients can rely on.
1. The Importance of Reliability in Medical Device Hardware
In the medical industry, embedded hardware reliability directly impacts patient health and safety. Any malfunction, no matter how minor, could lead to incorrect diagnoses, treatment delays, or even fatalities. Reliable embedded hardware ensures that medical devices operate continuously and accurately, providing healthcare professionals with the confidence to make critical decisions based on device data. Furthermore, reliability in these devices extends to long-term use, as they often operate in high-stress, real-time environments where performance cannot waver.
This emphasis on reliability also comes with regulatory scrutiny. Medical devices must comply with standards like ISO 13485 and IEC 60601 to ensure safety and efficacy. These standards focus on quality management and risk mitigation, reinforcing the need for rigorous design processes. The design must account for not only the function of each component but also how these components interact under diverse conditions.
2. Designing for Precision and Accuracy
Medical devices must produce precise and accurate results, as even the smallest error could lead to a misdiagnosis or ineffective treatment. Designers must carefully select high-quality components and thoroughly test them to ensure they meet the accuracy requirements. For example, imaging devices require embedded hardware that can handle complex algorithms and high data throughput without lag or error. Similarly, devices like insulin pumps or pacemakers demand pinpoint precision to deliver exact doses or maintain heart rhythms without deviation.
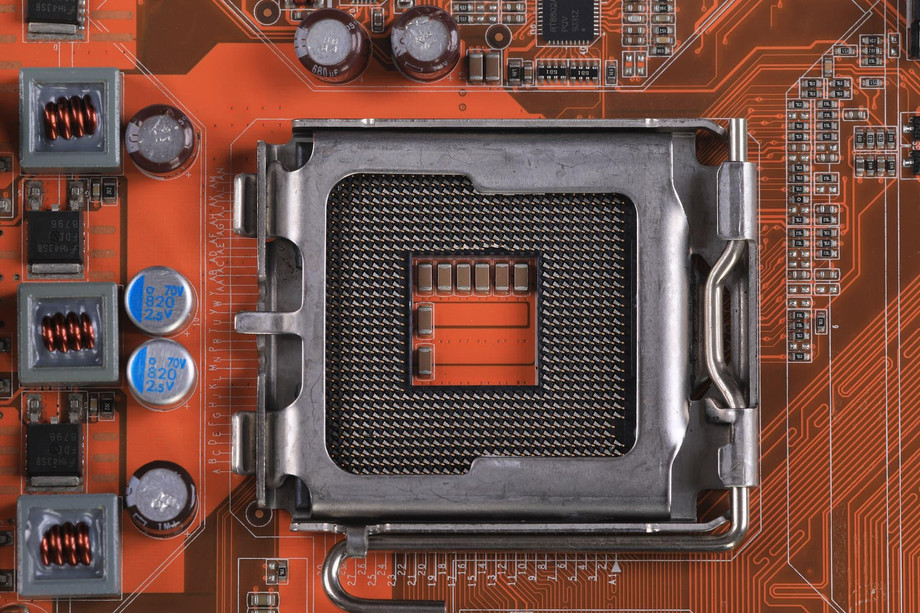
Achieving such precision often involves leveraging powerful microcontrollers, highly sensitive sensors, and precise analog-to-digital converters. It also requires a deep understanding of signal processing and noise reduction techniques to prevent any signal distortion or interference, which could impact the accuracy of the medical device.
3. Meeting Industry Standards and Regulations
Medical devices are subject to stringent regulatory standards to ensure they meet safety and performance criteria. Standards like ISO 13485 (Quality Management for Medical Devices) and IEC 60601 (Medical Electrical Equipment) provide guidelines for the development, testing, and production of medical devices. These standards mandate comprehensive testing for reliability, including environmental stress testing, failure mode analysis, and performance validation.
Designing for compliance requires collaboration with regulatory experts to ensure that every step, from initial design to final production, aligns with legal and industry standards. This process not only ensures that the product meets essential safety requirements but also helps streamline the path to market approval.
4. Prioritizing Cybersecurity in Embedded Hardware Design
In the digital age, cybersecurity has become a critical aspect of embedded hardware design, especially for networked medical devices that transmit sensitive patient data. Any breach in a medical device’s security could compromise patient information or, in extreme cases, allow unauthorized access to the device’s functions. For example, an internet-connected pacemaker must be equipped with robust encryption and authentication measures to prevent unauthorized access.
Incorporating secure boot processes, encrypted communication, and regular firmware updates are essential measures to protect medical devices from cyber threats. Furthermore, device designers should consider cybersecurity at the beginning of the design process rather than as an afterthought, as building secure systems from the ground up is far more effective than retrofitting security solutions later.
5. Power Management for Extended Device Operation
Many life-saving medical devices are either implanted or used in portable, power-sensitive applications, requiring embedded hardware that can operate effectively on limited power. This makes efficient power management a crucial consideration in the design of medical devices. By selecting components that consume minimal power and implementing energy-saving algorithms, designers can extend device battery life, which is essential for devices like pacemakers or wearable monitors that must operate continuously for extended periods.
Advanced power management features such as low-power modes, efficient energy storage, and adaptive power scaling are instrumental in maintaining the device’s operation while conserving battery life. These features ensure that the device can deliver consistent performance without frequent recharging or battery replacement, which is particularly critical for life-sustaining medical devices.
6. Ensuring Robustness in Extreme Conditions
Medical devices are often used in challenging environments where extreme temperatures, humidity, and physical stress can compromise their performance. Embedded hardware design for these devices must therefore account for these environmental factors to ensure reliability under all conditions. This includes selecting components with high tolerance for temperature variation, as well as using ruggedized materials that can withstand physical shocks and exposure to contaminants.
For instance, defibrillators and ventilators may be used in high-stress hospital environments or during emergency situations, where they are exposed to various stressors. In such cases, ruggedized and carefully designed embedded hardware ensures that these devices will function without fail, providing essential support when it matters most.
7. Testing and Validation: The Heart of Reliable Design
Testing and validation are at the core of designing embedded hardware for medical devices. Rigorous testing processes, including functional, environmental, and stress testing, are necessary to identify any potential weaknesses before the device reaches the market. Simulation tools allow engineers to test device performance under hypothetical conditions, revealing issues that may not appear in standard testing environments.
Moreover, real-time testing with live data ensures that the device can handle the types of signals it will encounter in real-world medical scenarios. Comprehensive testing protocols, often guided by regulatory standards, are indispensable in building reliable medical devices that meet both performance and safety requirements.
8. Leveraging Redundancy for Mission-Critical Applications
In life-saving medical devices, redundancy is a key design principle to ensure that the device continues to function even in the event of a hardware failure. By incorporating duplicate or backup systems, designers can create medical devices that maintain functionality in critical situations. For example, ventilators or dialysis machines might have redundant power supplies and processors to prevent downtime, providing peace of mind to both patients and healthcare providers.
This approach minimizes the risk of failure by allowing the device to switch to a backup system automatically if a primary component fails. Redundancy is a hallmark of robust medical device design, as it provides an additional layer of security for life-supporting equipment.
9. Trends in Embedded Hardware for Medical Devices
As technology evolves, new trends are emerging in the design of embedded hardware for medical applications. The integration of artificial intelligence (AI) and machine learning (ML) into medical devices is helping improve diagnostic accuracy and personalize patient care. Additionally, the adoption of flexible, wearable electronics is expanding the reach of medical devices, making monitoring and treatment more accessible and convenient.
Furthermore, the growth of IoT in healthcare is creating opportunities for connected medical devices that can communicate patient data in real-time to healthcare providers. This allows for proactive and responsive treatment, as medical staff can monitor patients remotely and intervene quickly if needed. As these trends continue to advance, the design and development of embedded hardware design will evolve, focusing on enhancing connectivity, miniaturization, and intelligence in medical devices.
To Know More About embedded hardware design