A large number of fraudulent activities in healthcare, increasing number of patients seeking health insurance, high returns on investment, and the rising number of pharmacy claims-related frauds. However, the dearth of skilled personnel is expected to restrain the growth of this market.
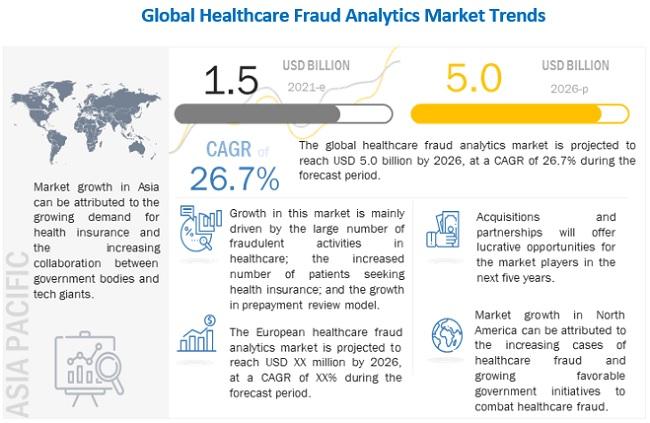
According to new market research report, "Healthcare Fraud Analytics Market by Solution Type (Descriptive, Predictive, Prescriptive), Application (Insurance Claim, Payment Integrity), Delivery (On-premise, Cloud), End User (Government, Employers, Payers), COVID-19 Impact - Global Forecast to 2026", is projected to reach USD 5.0 billion by 2026 from USD 1.5 billion in 2021, at a CAGR of 26.7% during the forecast period.
The public & government agencies segment accounted for the largest share of the healthcare fraud analytics market in 2019. The increasing cost burden due to healthcare fraud is proving to be a financial threat to public and government agencies globally. These factors are compelling payer organizations associated with these agencies to adopt analytics solutions to avoid losses incurred due to FWA and improper payments, which is driving the market growth.
The healthcare industry has been witnessing a number of cases of frauds, done by patients, doctors, physicians, and other medical specialists. Many healthcare providers and specialists have been observed to be engaged in fraudulent activities, for the sake of profit.
Download PDF Brochure @ https://www.marketsandmarkets.com/pdfdownloadNew.asp?id=221837663
Over the years, the number of people benefitting from various healthcare schemes has grown considerably. A couple of reasons contributing to the growth of the health insurance market include the rise in the aging population, growth in healthcare expenditure, and increased burden of diseases.
The healthcare industry is changing at an incredible rate, and one of the major contributors to this change is the increasing popularity of healthcare communication through social media.
The deployment of fraud analytics solutions is a time-consuming process. The process involves creating user interfaces, new databases, and predictive models; evaluating and deploying models, and monitoring their effectiveness. In this process, data analysts continuously run algorithms until they get the most effective predictive model.
