As medical devices become more advanced, the need for secure, reliable, and precise embedded hardware design has grown paramount. Medical equipment today not only performs critical health functions but also processes sensitive patient data, connecting to networks that need secure management. Designing embedded hardware for medical applications requires a nuanced understanding of security, precision, and compliance standards to meet the stringent demands of the healthcare sector.
This blog explores essential considerations and strategies to achieve secure embedded hardware design tailored for medical devices, ensuring reliability, data integrity, and compliance with global healthcare standards.
1. Importance of Security in Embedded Hardware for Medical Devices
The healthcare sector faces constant cyber threats as it increasingly relies on interconnected systems. From monitoring devices to complex diagnostic equipment, embedded hardware in medical applications must resist cyber-attacks to protect patient safety and privacy. Breaches can lead to dire consequences, not only risking patient data but also potentially disrupting life-saving functionalities of medical devices.
To safeguard devices against unauthorized access and tampering, hardware design must prioritize robust security measures. This involves implementing a secure boot process, encryption, secure communication protocols, and authentication mechanisms to prevent malicious interference at the hardware level. Security needs to be ingrained in the design phase itself, integrating hardware and firmware features that defend against evolving cyber threats.
2. Prioritizing Precision in Embedded Medical Devices
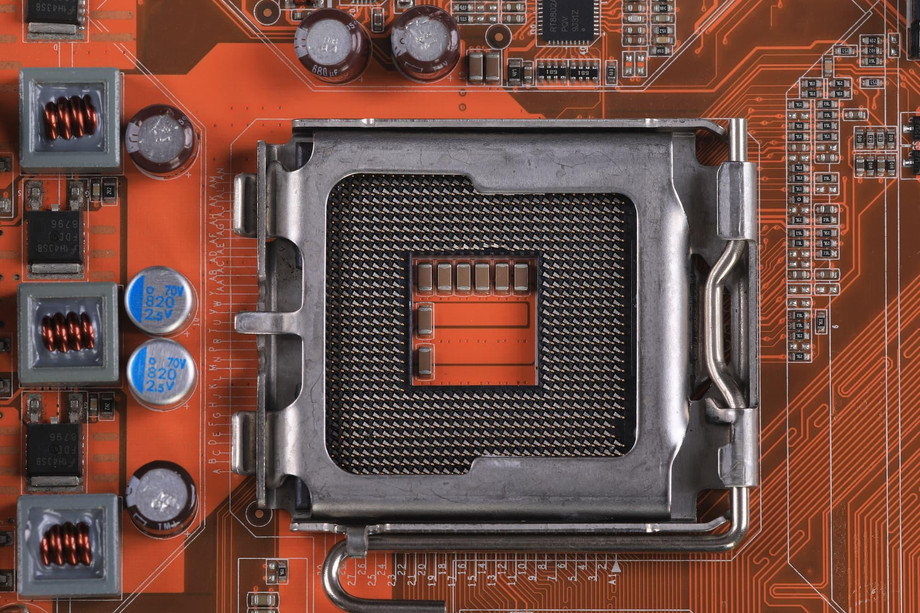
Precision in medical devices is non-negotiable. Devices such as infusion pumps, insulin pumps, and pacemakers must deliver exact, controlled doses to avoid fatal consequences. Embedded hardware is responsible for processing input from various sensors, performing real-time analysis, and executing precise outputs. Variations in any of these elements could compromise patient health.
To achieve this precision, developers utilize high-quality sensors and calibrated actuators, supported by microcontrollers with rapid processing capabilities. Designs must also take into account power management, as consistent power supply ensures the device operates accurately and reliably over time. Thus, embedded hardware for medical devices is meticulously engineered to deliver reliable and precise results, underpinned by robust quality control processes and regular calibration.
3. Regulatory Compliance and Certification Standards
Embedded hardware in medical devices is strictly regulated by entities such as the FDA (Food and Drug Administration) in the U.S., the European Medicines Agency (EMA), and other international regulatory bodies. These regulations exist to enforce rigorous safety, performance, and cybersecurity standards, ensuring the highest level of patient safety.
Key regulatory requirements include:
- FDA Approval and 510(k) Clearance: For devices intended for the U.S. market, the FDA mandates strict design controls, performance validation, and safety evaluations.
- IEC 60601-1 and IEC 62304 Standards: These international standards address the safety and essential performance of medical electrical equipment, ensuring robust design and reliable embedded hardware.
- HIPAA Compliance: While mainly applicable to data, HIPAA regulations affect hardware handling of sensitive patient data to ensure confidentiality and integrity.
- Cybersecurity Guidelines: The FDA and other regulators have issued cybersecurity recommendations specific to medical devices, urging manufacturers to integrate cybersecurity measures into embedded hardware design.
For manufacturers, meeting these standards is essential not only for legal market entry but also to establish trust with healthcare providers and patients. Compliance demonstrates that the device meets established safety and efficacy benchmarks, providing a foundation for widespread adoption and use.
4. Designing for Power Efficiency and Reliability
Medical devices often operate continuously or in remote environments, requiring highly efficient power management to maintain functionality. Power efficiency directly impacts device size, weight, and overall reliability—critical factors, especially in portable and wearable devices.
Strategies to enhance power efficiency in embedded hardware include:
- Low-power Microcontrollers (MCUs): Modern MCUs are designed to minimize power consumption, essential for battery-operated medical devices.
- Energy Harvesting Techniques: Certain devices utilize energy harvesting, capturing power from environmental sources (e.g., body heat or movement) to supplement or replace battery power.
- Power Optimization Algorithms: Advanced embedded systems implement power management algorithms that optimize energy consumption based on the device's state, extending battery life without sacrificing performance.
By incorporating efficient power solutions, embedded hardware design ensures reliable operation over extended periods, reducing maintenance and replacement needs, a significant advantage in clinical and personal healthcare settings.
5. Ensuring Data Integrity and Privacy in Embedded Medical Devices
Data integrity and privacy are crucial in medical devices where information accuracy can directly impact patient outcomes. Embedded systems must accurately collect, process, and transmit data, requiring robust error-checking and encryption protocols. This prevents data corruption during transfers and unauthorized access to patient information, which is critical to maintain trust and compliance with healthcare regulations.
To ensure data integrity:
- Secure Communication Protocols: Use encrypted communication protocols like TLS/SSL for data transmission between devices and medical databases.
- Error-detection and Correction Mechanisms: Implement redundancy checks (e.g., CRC or checksum) to validate data integrity during transfers.
- Data Logging: Devices should log data securely to provide a verifiable record of activity, which is essential for regulatory audits and diagnostics.
By safeguarding data privacy and integrity, medical devices maintain their reliability and align with global data protection laws, such as HIPAA in the U.S. and GDPR in Europe, assuring patients and providers of robust data security.
6. Building Secure Firmware and Software Interfaces
Firmware is central to an embedded system’s functionality, controlling how the hardware interprets input and delivers output. A secure firmware environment is fundamental to prevent vulnerabilities from being exploited, potentially compromising the device. Embedded hardware for medical devices requires firmware designed with security-first principles, such as secure boot, access controls, and frequent updates.
Approaches for secure firmware in medical devices include:
- Secure Boot: This process ensures that only authenticated firmware is loaded, blocking unauthorized code from running on the device.
- Access Controls and Authentication: Limiting device access to authorized users only, using multi-factor authentication when possible.
- Firmware Updates and Patching: Developing mechanisms for safe and reliable updates, allowing manufacturers to patch vulnerabilities as threats evolve without compromising device functionality.
Secure firmware is integral to achieving both security and reliability in medical devices, providing a fortified foundation for secure operation in sensitive healthcare environments.
7. Testing and Validation: Ensuring Precision and Security
Testing is a critical phase in embedded hardware development, ensuring the device meets strict regulatory and performance standards. Validation processes are necessary to verify that the embedded system operates securely and precisely under all conditions it might encounter in real-world use.
Testing protocols should include:
- Functional Testing: Ensures the device performs as expected, handling input and output accurately.
- Security Testing: Evaluates the system's resilience to potential security threats, identifying and addressing vulnerabilities.
- Compliance Testing: Confirms that the device meets industry standards like IEC 60601 for electrical safety and ISO 14971 for risk management.
Testing protocols allow developers to simulate real-world scenarios, providing assurances of reliability and security that align with both regulatory requirements and patient safety.
8. Future Trends in Secure Embedded Hardware for Medical Devices
The medical device landscape is evolving rapidly, with trends like AI integration, edge computing, and 5G connectivity transforming possibilities. Advanced medical devices increasingly rely on artificial intelligence to provide predictive insights or customize care. Edge computing enables data processing directly on the device, reducing latency and enhancing response time, while 5G connectivity offers faster and more reliable data transfer, crucial for devices used in remote monitoring or emergency care settings.
These advancements come with additional security and precision challenges. To support these technologies, embedded hardware design for medical devices will increasingly incorporate enhanced processing power, fortified security features, and advanced data management capabilities. Designers will need to balance innovation with the security and precision standards required in medical applications.
Conclusion
Designing secure and precise embedded hardware design for medical devices demands a multifaceted approach, balancing security, regulatory compliance, power efficiency, and data integrity. By integrating security from the ground up and adhering to rigorous testing and compliance standards, manufacturers can produce devices that not only perform with high accuracy but also protect patient data and safety. As technology evolves, so will the complexity of embedded hardware in healthcare, creating new opportunities for enhanced patient care and innovative medical solutions.
To Know More About embedded hardware design